Key concepts for epidemic response managers
To support or manage an epidemic response it is important to understand basic concepts of epidemiology. This section includes a list of basic principles of epidemiology and how or why certain terminologies or calculations should be used to inform epidemic prevention and response.
In the Disease Tools available for managers, you will frequently find the terms listed below. Further and more detailed information on these terms and on other key public health concepts is in the following section (2. Key Public Health Concepts).
A case definition is a set of uniform criteria used to define a disease for public health surveillance. It enables public health officials to classify and count cases consistently. Case definitions are used for surveillance purposes only - clinical diagnosis and treatment can be based on other criteria. During an epidemic, case definitions used for routine surveillance should be reviewed and modified if needed, to be more specific for the given epidemic and context. Note that these may change in an outbreak and it is important to adhere to the case definitions established by the Ministry of Health. Case definitions can refer to suspected, probable and confirmed cases or they can be clinical, epidemiological and laboratory case definitions.
An alert threshold is the pre-defined number of alerts that suggest the beginning of a possible disease outbreak and therefore warrant immediate notification. Every alert must be triaged, verified, risk assessed and deemed a response is needed.
Epidemic thresholds are the minimum number of cases indicating the beginning of a particular disease’s outbreak. Specific and non-specific epidemic thresholds have been defined for different diseases:
- Specific threshold: a single reported case can imply an outbreak, for example for measles, cholera, Shigella, yellow fever and viral haemorrhagic fever.
- Non-specific threshold: An increase above the expected number of cases for a particular population at a specified time of year in a defined location may indicate an outbreak. There is no specific threshold level to define malaria outbreaks for example.
Although there are some internationally recognized signals constituting an ‘alert’ in certain contexts, there are no globally established criteria and thresholds should be adapted based on the country and its context. Therefore, this website does not propose any thresholds, and managers are encouraged to check with national health authorities what the nationally recognised threshold may be for a specific disease.
Risk of getting a disease during a specific time period (such as during an outbreak). Can also be expressed as age or gender specific attack rate, which can tell you who is most vulnerable.
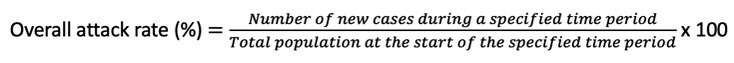
A secondary attack rate is sometimes calculated to document the difference between community transmission of the disease versus transmission of the disease in a household or among other closed population.
Infectious agents are bacteria, viruses, fungi, prions and parasites. A disease caused by an infectious agent or its toxic products is defined as an infectious disease. Infection occurs when the infectious agent establishes itself in the host individual and reproduces itself or some stages of its life cycle.
Vectors are living organisms that can transmit infectious agents between humans, or from animals to humans (mosquitoes, fleas, ticks, Triatomine bugs, rodents, snails etc.).
A reservoir of infection is a living organism or material in or on which an infectious agent lives and/or usually multiplies. Reservoirs include humans, animals and the environment. Human reservoirs may or may not show the effects of illness. The reservoir may or may not be the source from which an agent is transferred to a susceptible host.
A susceptible host is a person at risk of being infected. The level of susceptibility depends on age, sex, ethnicity, genetic factors, and specific immunity It also depends on other factors that affect an individual's ability to resist infection or to limit its ability to cause infection.
A zoonotic disease or zoonosis is an infectious disease disease that can be transmitted from animals to humans and from humans to non-human animals. It is estimated that, globally, about one billion cases of illness and millions of deaths occur every year from zoonoses. About 60% of emerging infectious diseases are zoonoses, and over 75% of new human pathogens detected in the last three decades are zoonotic.
Categorisation of modes of transmission varies from one agency to another. In addition, some infectious agents can be transmitted by more than one mode. The following is a list to serve as guidance to better understand the diseases included in this website.
- Airborne spread: This refers to the transmission of infectious agents through ‘droplet nuclei’. Unlike droplets that fall on the ground within a short distance, droplet nuclei can remain suspended in the air for a longer duration and can be blown over long distances. Droplet nuclei can be inhaled.
- Droplet spread: This is the spread of aerosols produced by coughing, sneezing or talking. Once expelled, droplets travel short distances and tend to fall rapidly on the ground or nearby surfaces. They can also be transferred to someone’s hand who may rub their eyes, nose or mouth.
- Contact transmission: Direct contact through skin-to-skin contact or contact with body fluids. This includes:
- Sexual transmission
- Congenital transmission: That is the vertical transmission from a mother to her new-born in utero or during delivery.
- Fecal-oral transmission: This is the transmission of pathogens of faecal particles from a person to the mouth of another person, by consuming contaminated food or water.
- Vector borne: Refers to the transmission through animals or insects that carry an infectious agent. Vectors are living organisms that transmit pathogens human-to-human or animal-to-human.
- Vehicle borne transmission: Refers to the indirect transmission of an infectious agent through inanimate objects such as water, blood, soil or fomites on objects such as bedding.
This time from when infection occurs to the onset of symptoms is called the incubation period. It is a range of days and it can be different for each disease.
The latency period (also known as the latent period or the pre-infectious period) is the time interval between when an individual or host is infected by a pathogen and when he or she becomes infectious, i.e. capable of transmitting pathogens to other susceptible individuals.
Period of infectiousness is the time interval during which an infected person can transmit the infection to other susceptible persons. It varies between diseases and it can include the incubation period, stage of clinical disease and the stage of recovery. During this infectious period, the aim of disease prevention and control is to limit exposure to the source either by using personal protective equipment, infection control measures, quarantine or isolation.
This website includes a section for vaccines and available treatments for each one of the Disease Tools included. It should be noted that the purpose is not to provide guidance on clinical management for any of the diseases. Instead, it is aimed at providing information to response managers on existing basic vaccine and treatment strategies . Health professionals should refer to the appropriate local or international guidelines for clinical management. All clinical management including the administration of a treatment or vaccine should be conducted by a health professional.
The precondition for an infection is the presence of a susceptible host. Theoretically, if the whole population is immune to an infection due to vaccination, the disease would be eradicated. However newborn babies would be susceptible, some people have contraindications and cannot be vaccinated, and the efficacy of vaccines is not 100%. As an example, one dose of vaccine against Measles is about 93% protective.
Nevertheless, the lower the proportion of susceptible hosts in population, the lower the possibility for occurrence of the infection. This is called herd immunity. A very high percentage of individuals in a population is immune, so the chance an agent will ‘find’ a susceptible host is very low. In other words, those who are immune ‘protect’ those who are not e.g. individuals with contraindications for vaccination
There are two types of immunity:
- Active immunity results when exposure to an agent triggers the immune system to produce antibodies to that disease. It may be natural active immunity (due to infection) and vaccine-induced immunity.
- Passive immunity is provided when a person is given antibodies to a disease rather than producing them through his or her own immune system. It may also be natural (a newborn baby acquires passive immunity from its mother through the placenta). A person can also get passive immunity through antibody-containing blood products such as immune globulin.
Each Disease Tool from this website includes a list of activities proposed and conceived for RCRC volunteers to take part on in their communities, in response to crises and epidemics. It should be noted that the proposed activities do not represent an exhaustive list of all prevention and control activities for a specific diseases. Importantly, proposed activities are conceived to be conducted in communities and outside clinical settings; therefore, the proposed interventions exclude clinical management activities.
Epidemiology is the study of disease distribution and its related determinants (e.g. risk factors, symptoms) and the application of this study to the control of diseases and other health problems. It is considered the basic science behind public health and tells us the WHO, WHAT, WHERE and WHEN of disease transmission.
 A disease caused by an infectious agent or its toxic products is defined as an infectious disease. Infection occurs when the infectious agent establishes itself in the host individual and reproduces itself or some stages of its life cycle.
A disease caused by an infectious agent or its toxic products is defined as an infectious disease. Infection occurs when the infectious agent establishes itself in the host individual and reproduces itself or some stages of its life cycle.
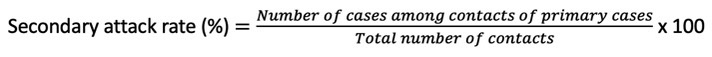
The transmission of infectious disease is described by a chain of six elements, or the chain of infection, that are needed for infection and disease to occur in an individual. Elimination of only one element of the chain of infection will interrupt disease transmission. This is the core principle behind epidemic prevention and control.
For some infectious agents, there are effective measures to interrupt the chain of transmission at more than one element. An example is yellow fever. Susceptible hosts can be protected with vaccination. Vector control methods can be used to limit the reservoir and block transmission such as screens and personal protection against mosquito bites.
For other infectious agents, measures towards all of the chain’s elements are less effective. For example, if the reservoir is unknown or it is an animal; the agent can be transmitted by air; or there is no vaccine available. Understanding the chain for specific diseases ensures we can break the cycle of transmission. For each epidemic it is important to know and identify each of the below.
|
Infectious agents are bacteria, viruses, fungi, prions and parasites. A minimum infective dose is required for an infection. Sometimes a few bacteria are sufficient to cause an infection (e.g. Shigella), but sometimes hundreds of thousands or millions are required (e.g. Vibrio cholerae). |
|
A reservoir of infection is a living organism or material in or on which an infectious agent lives and/or usually multiplies. Reservoirs include humans, animals and the environment. Human reservoirs may or may not show the effects of illness. The reservoir may or may not be the source from which an agent is transferred to a susceptible host. For example:
|
A zoonotic disease or zoonosis is an infectious disease that can be transmitted from animals to humans and from humans to non-human animals. It is estimated that, globally, about one billion cases of illness and millions of deaths occur every year from zoonoses. About 60% of emerging infectious diseases are zoonoses, and over 75% of new human pathogens detected in the last three decades are zoonotic. It represents a major public health problem around the world due to a close relationship with animals in agriculture, as companions and in the natural or wildlife environment. They also have far-reaching impacts and consequences on the economies and livelihoods of people and communities
A person with asymptomatic infection (a person is infected, but there is no symptoms) who can transmit the agent to others, is called a carrier. They can be:
- Healthy carriers: those who never experience symptoms, despite being infected
- Convalescent carriers: those who have recovered from their illness but remain capable of transmitting to others; or
- Chronic carriers.
| Portal of exit is the path by which the infectious agent leaves the host. It usually corresponds to the site where the pathogen is localized. The portal of exit can be the respiratory tract (coughing, sneezing, kissing), genitourinary tract (urine, semen, vaginal secretion), gastrointestinal tract (stool) or through skin or the placenta. |
|
There are many ways in which disease can spread. Understanding the source of infection and how it is transmitted is key in being able to prevent and control epidemics. First, the infectious agent leaves the host (exit). There are many routes of transmission that allow diseases to spread. Routes include through the respiratory tract (coughing, sneezing, kissing), genitourinary tract (urine, semen, vaginal secretion), gastrointestinal tract (stool), through skin or the placenta. |
Direct or indirect transmission of the infectious agent from its reservoir to a susceptible host can occur:
- Direct transmission includes direct contact (skin-to-skin contact, kissing, sexual intercourse) and droplet spread (aerosols produced by sneezing, coughing, talking). The source is an infected person.
- Indirect transmission may be airborne (infectious agents are carried by dust or are suspended in air), vehicle-borne (food, water, blood and other biological products, objects) and vector-borne (insects). The source of infection can be a person. It can also be contaminated or infected foods, animal vectors and reservoirs or different materials in the environment such as water and soil.
| The portal of entry is the way an infectious agent enters a susceptible host. It can be respiratory tract (inhaling germs or kissing), mouth (food or water ingestion), skin (insect bites, cuts), mucous membrane (e.g. contact of eye with dirty hands), the blood (transfusion, needle-sharing) and trans-placental mode of entry. |
The table below provides some examples of different reservoirs, portals of exit and entry, and mode of transmission.
Example different reservoirs, portals of exit and entry and mode of transmission
| Disease (agent) | Reservoir | Portal of exit | Mode of transmission | Portal of entry |
|---|---|---|---|---|
| Cholera (Vibrio cholera) | Humans | Gastrointestinal tract | Water | Mouth |
| Malaria (Plasmodium) | Humans | Blood-sucking mosquitos | Vectors (mosquitos) | Bite of mosquitos |
| Poliomyelitis (Polio virus) | Humans | Gastrointestinal tract | Water, person-to-person | Mouth |
| Hanta pulmonary syndrome (Hantavirus) | Animals (rodents) | Urinary tract | Airborne | Respiratory tract |
| A susceptible host is a person at risk of being infected. The level of susceptibility depends on age, sex, ethnicity, genetic factors, and specific immunity It also depends on other factors that affect an individual's ability to resist infection or to limit its ability to cause infection. For example, Hepatitis A is usually asymptomatic in children and can be severe in adults, and Polio is mostly severe in children. |
This time from when infection occurs to the onset of symptoms is called the incubation period. It is a range of days and it can be different for each disease. The incubation period duration will vary depending on the:
- Mode of transmission e.g. shorter for foodborne and longer for waterborne,
- Portal of entry e.g. Tetanus or Rabies will have a shorter incubation time if the wound is on the head; and
- Immune status of the susceptible person.
Knowing the incubation period is important in controlling epidemics. It helps identify who else may be infected, when and how control measures should be implemented, and helps in estimating the number of people that could get sick.
Period of infectiousness is the time interval during which an infected person can transmit the infection to other susceptible persons. It varies between diseases and it can include the incubation period, stage of clinical disease and the stage of recovery. During this infectious period, the aim of disease prevention and control is to limit exposure to the source either by using personal protective equipment, infection control measures, quarantine or isolation.
The precondition for an infection is the presence of a susceptible host. Theoretically, if the whole population is immune to an infection due to vaccination, the disease would be eradicated. However newborn babies would be susceptible, some people have contraindications and cannot be vaccinated, and the efficacy of vaccines is not 100%. As an example, one dose of vaccine against Measles is about 93% protective.
Nevertheless, the lower the proportion of susceptible hosts in population, the lower the possibility for occurrence of the infection. This is called herd immunity. A very high percentage of individuals in a population is immune, so the chance an agent will ‘find’ a susceptible host is very low. In other words, those who are immune ‘protect’ those who are not e.g. individuals with contraindications for vaccination
There are two types of immunity:
- Active immunity results when exposure to an agent triggers the immune system to produce antibodies to that disease. It may be natural active immunity (due to infection) and vaccine-induced immunity.
- Passive immunity is provided when a person is given antibodies to a disease rather than producing them through his or her own immune system. It may also be natural (a newborn baby acquires passive immunity from its mother through the placenta). A person can also get passive immunity through antibody-containing blood products such as immune globulin.
Passive immunity provides immediate protection from a specific disease, but it lasts only from a few weeks to a few months. In contrast, active immunity usually takes several weeks to develop, but it lasts much longer, and for some diseases it is a life-long.
Vaccines are biological preparations that improve immunity to a disease. A vaccine typically contains an agent that resembles a disease-causing microorganism. It is often made from a weakened or killed form of the microbe, its toxins or one of its surface proteins. The agent stimulates the body's immune system to recognize the agent as foreign, and subsequently destroy it and "remember" it so it is destroyed on any additional encounters.
Some of the numerous vaccines available worldwide are part of a routine immunisation programme. The World Health Organisation (WHO) makes recommendations for the routine immunisation and each country decides which vaccines will be included in the national immunisation programmes. This decision is usually made based on a country’s health priorities, epidemiological situation, available health workforce, logistics (including ‘cold chain’) and financial sustainability. The WHO recommendations can be found here: http://www.who.int/immunization/policy/Immunization_routine_table1.pdf
Besides routine vaccination, vaccines can be used as in epidemic control, for international travellers or for some epidemiological (for individuals more exposed to an agent) or clinical reasons (for individuals who suffer from a disease that make them more vulnerable to another disease that can be prevented by vaccination).
Vaccine safety is particularly important as safety failure can cause severe damage to health of individuals and to the entire immunisation programme. Vaccine side effects may be results of the vaccine itself, but also a result of unsafe vaccination practices.
The purpose of the vaccine ‘cold chain’ is to maintain product quality from the time of manufacture until the point of administration. It ensures that vaccines are stored and transported within the WHO-recommended temperature ranges.
Detecting new outbreaks early and understanding where they are and who they are affecting is critical in preventing the spread of the epidemic.
In the context of epidemics, surveillance is the continuous, systematic collection, monitoring, analysis and interpretation of data related to communicable diseases. It is needed for the detection of epidemics, prompt and adequate response, and the planning, implementation, and evaluation of public health practice. Surveillance data tells us who is affected and where the disease is occurring.
- Early Detection: to serve as an early warning system for impending public health emergencies (outbreaks) and support rapid response;
- To document the impact of an intervention (e.g. immunisation), or track progress towards specified goals; and
- To monitor and clarify the epidemiology of communicable diseases, to allow priorities to be set and to inform public health policy and strategies.
Useful links:
www.cbsrc.org<
https://www.ifrc.org/document/community-based-surveillance-guiding-principles
There are different types of surveillance including:
- Indicator-based surveillance (IBS), which is the systematic collection, monitoring, analysis and interpretation of structured data (disease specific indicators) produced by health facilities or well-identified other sources (such as trained volunteers or community health workers).
- Event-based surveillance (EBS), is the organized collection, monitoring, assessment and interpretation of primarily unstructured or ad hoc information regarding potential public health hazards, which may represent an acute risk to human health. EBS can take place both at the facility and community level, and does not include disease specific data, but can be used to help identify newly emerging, or re-emerging diseases otherwise not included in traditional surveillance. Examples include CBS, hotlines, or unusual events at the facility level.
- Routine or passive surveillance, which is usually based on mandatory regular disease reporting inside a health system, which can include both facility and community-based surveillance strategies, and is often linked to ongoing or existing health activities. It is part of the IBS.
- Active surveillance, when each reported case of a disease is further investigated. Often it requires negative reporting (i.e. reporting that there was no case of a disease registered), and may include active case finding.
- Community-based surveillance (CBS) – is the systematic detection and reporting of events of public health significance within a community by community members. In the Red Cross and Red Crescent Membership this is done through volunteers who are trained to recognize and report on health risks and unusual events to ensure communities receive the support they need at the right time and place.
- Sentinel surveillance - a ‘sample surveillance’ where only a selected group (e.g. specific health workers, or specific health facilities) are involved to collect a sample of data that is generalizable to the population
- Laboratory-based surveillance.
- One Health/Collaborative Surveillance - One Health is a collaborative and multisectoral approach combining environmental, animal and human health to achieve better public health outcomes. This surveillance framework is an emerging one that seeks to foster multisectoral joint surveillance and information sharing across human, animal and environmental health sectors. This will help to better understand disease drivers in the animal and environmental health, enhance early warning systems (especially before disease spread to humans), and strengthen preparedness and response to outbreaks.
Communicable disease surveillance is usually organised on international, national or sub-national level. The National Ministries of Health and public health institutions/centres for disease control and prevention, are responsible for these surveillance systems. Surveillance should be conducted for both human and animal diseases.
An important element of surveillance is disease (or syndrome, condition, risk factor, agent) reporting. Health institutions, laboratories and health professionals i.e. ‘surveillance units’, report them to the central or intermediate level. This is where the information on registered disease is analysed and interpreted for both human and animal health. Surveillance findings are used as a trigger for public health measures.
A case definition is a set of uniform criteria used to define a disease for public health surveillance. It enables public health officials to classify and count cases consistently. Case definitions can be case-based and syndrome-based.
Case-based definitions are usually based on the individual data of a patient, and epidemiological or laboratory confirmation. The main objective of syndrome-based definitions is to identify illness clusters early, before diagnoses are confirmed and reported to public health agencies. This allows the mobilization of a rapid response, thereby reducing morbidity and mortality.
Case definitions are used for surveillance purpose only - clinical diagnosis and treatment can be based on other criteria. During an epidemic, case definitions used for routine surveillance should be reviewed and modified if needed, to be more specific for the given epidemic and context. CBS is an example of a type of surveillance that uses syndrome-based definitions for detection.
Case definitions can refer to suspected, probable and confirmed cases or they can be clinical, epidemiological and laboratory case definitions, as shown in the table below.
| Case | Definition |
|---|---|
| Suspected case | Usually a case that meets clinical criteria (symptoms of a disease) |
| Probable case | Includes clinical and epidemiological criteria, for example close contact of a case |
| Confirmed case | Includes laboratory confirmation of the disease |
Suspected case - Any person with acute onset of fever, with jaundice appearing within 14 days of onset of the first symptoms.
Probable case - A suspected case; and one of the following:
- presence of yellow fever IgM antibody in the absence of yellow fever immunization within 30 days before onset of illness; or
- positive postmortem liver histopathology; or
- epidemiological link to a confirmed case or an outbreak.
Confirmed case - A probable case;
And absence of yellow fever immunization within 30 days before onset of illness; and one of the following:
- detection of yellow fever-specific* IgM; or
- detection of fourfold increase in yellow fever IgM, or IgG antibody titres between acute and convalescent serum samples, or both; or
- detection of yellow fever-specific* neutralizing antibodies.
or
Absence of yellow fever immunization within 14 days before onset of illness; and one of the following:
- detection of yellow fever virus genome in blood or other organs by PCR; or
- detection of yellow fever antigen in blood, liver or other organs by immunoassay; or
- isolation of yellow fever virus.
Understanding and using terminology correctly is very important in epidemic prevention and control. Several terms are used to describe disease and their occurrences in a population. These terms are presented in the table below.
| Term | Explanation | Example |
|---|---|---|
| Absence of disease | No cases of a disease have been registered during a shorter or longer period | Yellow fever is absent in areas without Aedes and Haemagogus species (Europe, Asia, North America, Oceania) |
| Sporadic occurrence | Cases of a disease occur infrequently and irregularly | A single case of a disease or several unlinked cases during a longer time period |
| Endemic | A permanent presence of a communicable disease in a population. The number of cases of disease that occur each year is similar, with small fluctuations (except in situation where prevention and control programmes lead to reduction of the number of cases) | Cholera is endemic in approximately 50 countries in South and South-East Asia, Africa and Hispaniola. |
| Hyper-endemic | Persistent, high levels of disease occurrence | Meningococcal disease is hyper-endemic in Sub-Saharan Africa |
| Cluster | An aggregation of cases grouped in place and time, that are suspected to be greater than the number expected | Several cases of diarrhoea have been diagnosed in a few days in a community, with the number being higher than usual. It could be an outbreak and it must be investigated (another reason could be an artificial increase because of better reporting) |
| Outbreak |
An occurrence of an infection in a population with an excess of cases that would normally be expected in a defined community, geographical area or season. Outbreaks can occur in endemic areas: if significantly more cases of a disease have occurred than usual. Outbreaks can occur in areas where the disease was absent – in this situation even two linked cases can constitute an outbreak. A single case of a communicable disease long absent from a population or caused by an agent (e.g. bacterium or virus) not previously recognized in that community or area, or the emergence of a previously unknown disease, may also constitute an outbreak. |
Yellow fever outbreak after the disease had been imported from another country
A foodborne outbreak after exposure to a common source |
| Epidemic | A larger outbreak that affects a considerable proportion of a population. | Ebola epidemic in Western Africa 2013-2016 |
| Pandemic | An epidemic that has spread over several regions or continents, usually affecting many people. | COVID-19 |
Some other key definitions to understand for disease occurrence include:
Disease control: the reduction of disease frequency and its consequences to an acceptable level as a result of deliberate efforts.
Elimination of a disease: occurs if there is no natural circulation of a pathogen any longer in a population.
Eradication: this is reached if a pathogen does not circulate at all any more in the human population. An example is Smallpox, as described in the textbox below.
| Example of Disease eradication: Smallpox |
|---|
| Smallpox is the only infectious disease for which eradication has been achieved at present. The last case of Smallpox was isolated in October 1977, and the disease was certified as being eradicated in 1979. Several facts allowed Smallpox eradication: the disease was highly visible, as patients develop a rash that is easily recognized. In addition, the time from exposure to the initial appearance of symptoms is short, so that the disease usually can’t spread very far before it’s noticed. Further, only humans can transmit and catch Smallpox, and those who survived the disease naturally develop a lifelong immunity against further infection. For everyone else, vaccination was highly effective. |
Surveillance of communicable diseases is based on the measurement of disease occurrence. Monitoring the trends in the disease incidence rate allows the epidemic thresholds to be estimated. It also allows the monitoring of the disease incidence rate, mortality rate and case-fatality ratio, enabling the evaluation of the prevention and control effectiveness. However, surveillance measurements only include cases of disease that were diagnosed and reported – often the real number may be much higher, especially in difficult contexts e.g. if people die at home or in communities and are not registered.
The table below provides a summary of commonly used measurements in epidemics, including how they can be used in epidemic prevention and response to guide programming.
| Measurement | Definition and how to calculate it | How is it useful or used? |
|---|---|---|
| Crude mortality rate (CMR) |
Rate of death (from all causes) in an entire population. CMR = Deaths / (Population at risk x Period of time) x 10,000 = Deaths / 10,000 persons / day |
To assess and monitor how severe the situation is Commonly used threshold for decision making and planning (e.g. if scale up is needed) |
| Under 5 mortality rate (U5MR) |
Rate of death (from all causes) in children under 5 years old. U5MR = Deaths in children under 5 / (Number of children under 5 at risk x Period of time) x 10,000 = Deaths / 10,000 children under 5 years / day
|
To assess and monitor how severe the situation is Commonly used threshold for decision making and planning (e.g. if scale up is needed) More sensitive than CMR; use U5MR if baseline mortality is unknown or doubted |
| Disease-specific mortality rate |
Rate of death for a specific disease (e.g. measles or cholera). Disease specific MR = Deaths from the disease / (Population at risk x Period of time) x 10,000 = Deaths / 10,000 persons / day |
Can compare current mortality rate with previous epidemics or other diseases (or baseline / endemic mortality rate for that disease) Monitoring progression of an epidemic |
| Incidence rate (IR) |
Number of new cases of a disease during a specific time period, in a population who are at risk of the disease. IR = New cases of disease / (Population at risk x Period of time) x 1,000 persons = New cases due to specific disease / 1,000 persons / week (or month) |
Monitoring progression of an epidemic Used to calculate estimations of how many people could become infected
|
| Case fatality rate (CFR) |
The proportion of cases of a disease that result in death. In other words, the rate of death in people who have the disease.
CFR = Deaths due to the disease / Total cases of the disease x 100 = % |
Monitoring progression of an epidemic Monitor if interventions are working or are effective, especially case management (e.g. is CFR reducing?) Can compare with previous epidemics |
| Attack rate |
Risk of getting a disease during a specific time period (such as during an outbreak). Can also be expressed as age or gender specific attack rate, which can tell you who is most vulnerable. Attack rate = Number of cases during the outbreak / Total population at the start of the outbreak x 100 = % |
To calculate the expected number of cases during the current epidemic, to plan the scale of intervention, resources needed etc. To predict the magnitude of future epidemics of the disease |
| Basic reproductive ratio (R0) (or basic reproduction number) |
R0 must be estimated, reported, and applied with great caution because this basic metric is far from simple. R0 is rarely measured directly, and modelled R0 values are dependent on model structures and assumptions. Some R0 values reported in the scientific literature are likely obsolete. |
The basic reproduction number (R0), also called the basic reproduction ratio or rate or the basic reproductive rate, is an epidemiologic metric used to describe the contagiousness or transmissibility of infectious agents. R0 is affected by numerous biological, socio-behavioural, and environmental factors that govern pathogen transmission. R0 is not a biological constant for a pathogen, a rate over time, or a measure of disease severity, and R0 cannot be modified through vaccination campaigns. |
The officially declared status of an outbreak is not only important to determine prevention and control actions, but it also affects social, economic, political and security sectors of a country. Governments – ministries of health, local health authorities, or other authorities – have the power and mandate to declare an outbreak of an epidemic disease. National Societies should not declare outbreaks, but can nonetheless provide appropriate community-based health responses to suspect epidemic diseases, whether an outbreak is declared or not.
An early declaration of an outbreak by health authorities can allow for a faster public health response and boost financial support as relevant sectors activate response actions. A declaration may also change certain procedures to facilitate control. To give an example, the World Health Organization (WHO) recommends that once a cholera outbreak is declared, there is no need to confirm in a laboratory all suspected cases and instead, any person presenting with or dying from acute watery diarrhoea should be registered and reported as a suspected case. The declaration of an outbreak can facilitate importation procedures for necessary medication and equipment or speed the travel of investigators to understand the cause of a disease, if needed.
A declaration of a pandemic is the responsibility of the World Health Organization (WHO) and will normally trigger health authorities around the world to take a range of public health measures. From establishing the use of face masks in public places, for instance, to other more drastic measures such as restrictions on international travel or trade.
Criteria to declare an outbreak, epidemic or pandemic will depend on the type of disease and the authorities (e.g., Ministries of Health) or institutions (e.g., World Health Organization) providing technical guidance for outbreak control. For instance, in the case of cholera the Global Task Force on Cholera Control establishes that if at least one sample tests positive by culture and/or polymerase chain reaction (PCR), an outbreak should be declared, and control measures should immediately follow.
A declaration by a government authority may boost funding at a domestic level, e.g., from the national government to local authorities for control and response measures; or at an international level when funding flows from international organizations and donors. In places with limited access to health services and poor infrastructure, an epidemic declaration may be perceived as an ‘opportunity’ to bring in not only funding, but other much needed infrastructure to address the underlying causes of a disease. Managers should be aware of communities potentially misreading a situation of high risk to the health of the population as a chance for benefits that may be unrealistic or unfeasible without outbreak declaration. This is often the case of cholera outbreaks that may be perceived as an opportunity to bring in jobs, training and/or water and sanitation infrastructure. While some of these benefits may in fact follow a declaration, they are often temporary. Long-lasting improvements depend on technical skills and supervision over an extended period, continued public support and adequate budgets available. National Societies should be advocates of prevention activities rather than supporting a narrative that is reliant on epidemic crises to enhance change.
On another hand, an important factor to consider is that governments may at times fear that a formal declaration of an outbreak could negatively impact important sectors for the economy such as trade or tourism, or that the declaration may create an image of a country that has failed to provide basic services to its population (e.g., clean water and sanitation in the case of water-borne diseases). Such factors may lead authorities to delay the declaration or to not declare an outbreak altogether, e.g. in 2008 then-president Robert Mugabe declared “there is no cholera” despite an outbreak of over 16,000 cases in Zimbabwe. Other consequences may include sanctions on health workers or the media when reporting about the situation or even when mentioning the name of the epidemic disease. For instance, although cases in a community may meet the case definition for cholera, a government may be reluctant to declare an epidemic and may also unwelcome the use of the word “cholera”. Cholera is a type of Acute Watery Diarrhoea (AWD), and humanitarian actors working in such contexts may have to speak of cases of AWD if health authorities have not confirmed the presence of cholera.
This causes difficulties for the health system to manage caseloads, delays international supply chains of medication, and undermine coordination efforts and information-flow among responding actors, among other obstacles. Working in such circumstances can be particularly challenging for National Societies who are willing to act for the well-being of their communities but also support and adhere to the policies of the governments to which they are auxiliary.
The following are some general guidance pointers for managers. An understanding of the specific context is necessary to assess their relevance:
- Beware of the language that is used to describe the disease to minimize conflict and to maintain the necessary humanitarian space.
- Ensure that volunteers understand the symptoms for the disease of concern and continue supporting the early identification and referral of potential cases to health facilities. Prevention and response actions relevant during a low alert level of surveillance continue to be relevant and therefore volunteers can be able to continue them, albeit on a smaller scale than may be desired.
- Gather information from various reliable sources to understand the epidemiological situation and discuss it with regional IFRC offices in case funds are needed, but which may be more difficult to mobilize without an official declaration.
- Ensure that communities and volunteers understand that a declaration of the beginning (or end) of an outbreak are often politically charged decisions that affect how various actors will respond. Managers should identify key actors in the response sectors, from surveillance to case management, and ensure that information flows in as much as possible.
- Communicate to logistics teams that the importation of certain materials may be a challenge, and this should be considered in procurement timelines.
Defining the end of an outbreak requires an estimation of the risk of cases arising in the future using objective quantitative methods. The end of an outbreak helps health authorities to downgrade the alert level of surveillance efforts, reallocate health care resources to cover other health issues, restore health care workers regular work shifts, and start recovery efforts.
Just as with the declaration of the beginning of an outbreak, criteria to declare its end will depend on the type of disease and the authorities providing technical guidance. In the context of an Ebola Virus Disease (EVD) outbreak, for example, the end is declared following 42 consecutive days (i.e., twice the longest incubation period) of no cases recorded since the outcome of the last case detected. The outcome is defined as the second PCR negative test of blood samples or a safe burial if the person died. Another example of a criterion established during the 2017-18 cholera outbreak in South Sudan was no new cases reported for seven weeks.
The declaration of the end of an outbreak and of the criteria used however, can be problematic for various reasons and managers should be alert for potential issues. For instance, possible case flare ups through less common transmission routes, e.g., sexual transmission for EVD; through underreported cases due to limited or poor surveillance systems; or through asymptomatic cases. A recent study (Bimandra et al., 2021) showed that using the current WHO criteria to declare the end of an EVD outbreak, might be too short and too sensitive to underreporting.
For a wide range of diseases, National Societies can play a key role on supporting community-based surveillance activities during and after the official end of an outbreak to identify potential cases, even after the declaration of the end of an outbreak (See: https://www.cbsrc.org/).
Coordination between different Sectors
- Coordination between agencies and different sectors including WASH, Health, Nutrition and Shelter. For zoonotic disease outbreaks, coordination should include with animal and environmental health sectors.
- Coordination of volunteers.
Coordination between Agencies
- Camp Coordination and Camp Management – United Nations High Commissioner for Refugees (UNHCR) for conflict Internally Displaced Persons (IDP) and International Organization for Migration (IOM) for disaster situations.
- Protection - UNHCR for conflict IDPs and UNHCR/OHCHR/UNICEF for disasters and civilians affected by conflict other than IDPs.
- In refugee settings UNHCR also works in advocating and/or support efforts to improve access to healthcare; MHPSS services; sexual and reproductive health and HIV; nutrition and food security; and health information management.
- Emergency Shelter - UNHCR and IFRC.
- Health – World Health Organization (WHO).
- Emergency Telecommunications – World Food Programme (WFP).
- Logistics – WFP: WFP may be involved in in-kind food distribution or food aid via cash transfers in humanitarian settings, including disease outbreaks.
- Education – United Nations Children’s Fund (UNICEF) and Save the Children.
- Nutrition/UNICEF: UNICEF may also support countries to put in place measures to strengthen child- and newborn-health components in emergency preparedness plans, to minimize the risk of gender-based violence and to deploy human resources to affected areas. UNICEF also provides medicines, vaccines and other health supplies to children and women.
- Early Recovery – United Nations Development Programme (UNDP).
- Coordination – United Nations Office for the Coordination of Humanitarian Affairs (OCHA).
- One Health – Food and Agriculture Organization (FAO), World Organization for Animal Health (WOAH), and United Nations Environmental Programme (UNEP)