Poliomyelitis (polio)
Poliomyelitis (polio)
Last update: 2024-05-24
What’s on this page:
Key facts
Transmission: faecal-oral route
- Touching the mouth with hands or objects (for example, toys) that are contaminated by the faeces of a person infected with polio
- Drinking water or food contaminated by the faeces of a person infected with polio
Most vulnerable to severe consequences
- Children under the age of five years who are not vaccinated are most at risk
Most vulnerable to contracting the disease
- Unvaccinated people (especially children) living in areas with poor hygiene, sanitation and water infrastructure and services
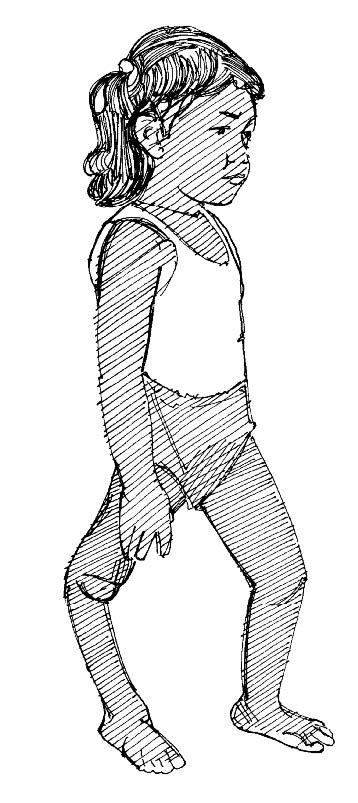
Acute flaccid paralysis (AFP) is a syndrome that can result from various diseases but is of major concern in cases of polio.
Symptoms of AFP
- Sudden loss of reflexes (movement)
- Severe muscle aches or weakness
- Loose and floppy arms and legs
- Difficulty breathing
Other polio symptoms
- Fever
- Tiredness
- Headache
- Vomiting
- Stiffness of the neck or back
- Pain in the arms or legs
What can you do to prevent and control an epidemic?
Monitoring the community and identifying sick people
- Identify possible source or point of contamination
- Identify community members with suspected polio and/or AFP according to the community case definition
Treatment and management
- Refer suspected cases to health facilities
- Promote routine vaccination against polio
- Provide psychosocial support to the sick person and their family members
Sanitation and waste management
- Promote use of appropriate sanitation and waste facilities (toilets/latrines)
- No open defecation
- Promote use of appropriate sanitation facilities (sound, clean latrines that are well maintained and have proper faecal sludge management)
Hand hygiene
- Promote good hand hygiene (handwashing with soap)
- BEFORE: preparing food; eating; feeding a child; treating wounds; or caring for sick people
- AFTER: using the toilet or cleaning a baby; touching garbage or waste; touching or feeding animals; blowing nose, coughing or sneezing; treating wounds; or caring for sick people
Food and water hygiene and safety
- Promote safe, clean drinking water store water in clean, covered water container
- Encourage exclusive breastfeeding for the first six months of life, and complementary breastfeeding until the age of two years (especially when a child is sick)
Social mobilization and health promotion
- Find out the specific advice being given by health and other relevant authorities
- Model following this advice and inform community members of current health practice advice
- Offer support and encouragement to follow the advice
- Try to gain understanding about if and why health practice advice is not being followed
- With the guidance of your supervisor and health authorities, work with communities to overcome barriers to following health advice and recommended practices
Immunization
- Support routine vaccination
- Support mass vaccination campaign
Mapping and community assessment
- Make a map of the community.
- Mark the following information on the map:
- How many people have fallen sick with acute flaccid paralysis (AFP)? Where?
- How many people have fallen sick with other symptoms of polio? Where?
- How many people have died? Where? When?
- Who and where are the vulnerable people?
- Where are the local health facilities and services? (include traditional healers)
- Record the following information on the back of the map:
- When did people start to fall sick with polio?
- How many people live in the affected community?
- How many are children under give years?
- Are children in the affected community vaccinated against polio?
- Approximately how many are not?
- What prevents people from vaccinating their children against polio?
- Have the health services been alerted to a potential polio case?
- Is a vaccination campaign planned?
- Where are community water sources?
- Are the water sources safe?
- Do people know how to treat water?
- How do they do it?
- What sanitation facilities are available? (put communal toilets/latrines on map)
- Do people use them?
- What handwashing facilities are available? (put handwashing stations on map)
- Do they have soap?
- What are the community’s habits, practices and beliefs about vaccinations? Are there societal, cultural or religious beliefs that prevent people from getting vaccinated?
- What are the community’s habits, practices and beliefs about caring for sick people? Consider any differences in roles and responsibilities between women and men.
- When babies and infants are sick, do women continue to breastfeed them?
- Is a social mobilization or health promotion programme in place?
- What are the roles, responsibilities, specific needs and priorities of women and girls, men and boys, and people with disabilities in handling, storing and treating water? Make sure you think about cultural and social traditions and perceptions, household decision-making, livelihoods such as agriculture and livestock raising etc.
- What are the barriers people face in accessing water points and sanitation and hygiene facilities, of all gender identities, ages, disabilities and backgrounds?
- Which sources do people use/trust the most for information?
- Are there rumours or misinformation about polio or the vaccine? What are the rumours?
A child with acute flaccid paralysis (AFP)
Volunteer actions
01. Community-based surveillance
02. Community mapping
03. Communicating with the community
04. Community referral to health facilities
05. Volunteer protection and safety
19. Mental Health and Psychosocial support (MHPSS)
24. Routine vaccinations
25. Mass vaccination campaigns
29. Hygiene promotion
30. Clean, safe household water
31. Good food hygiene
32. Sanitation
33. Encouraging the use and maintanace of latrines
34. Handwashing with soap
43. Social mobilization and behaviour change