Session 1.4. Special issues in dealing with epidemics and infections
By the end of this session, you will be able to:
- Discuss why epidemics can occur after natural disasters.
- Explain how to deal with dead bodies to prevent epidemics.
- Describe the One Health approach.
Part 1.4.1. Disasters and epidemics
Natural disasters happen frequently in many parts of the world and usually have a devastating effect on people and their property. They cause many deaths and injuries and rates of sickness also increase. They also cause people to move away from their destroyed homes and towns.
Different types of natural disaster affect communities in different ways. Some, such as earthquakes, cause many deaths and injuries and force many people to move. Others, such as floods or droughts, generally cause fewer deaths and injuries but frequently affect local crops and the availability of food and safe water.
To understand how infections and epidemics occur and develop during and after natural disasters, we need to understand how the impacts of natural disasters enable different types of epidemic to develop more easily. We will begin by looking at the effects of natural disasters on communities.
As we have noted, disasters can create conditions that help epidemics to spread. Many epidemics, such as diarrhoeas and respiratory infections, are very likely to occur after natural disasters; others, such as malaria, can sometimes occur.
To understand these effects, we need to remember what helps spread epidemics.
Participate
Name some of the kinds of natural disasters that you know about and say what effects they can have on people and communities.
It is often more challenging to deal with epidemics after a natural disaster than in other situations. This is because disasters often affect the ability of clinics and hospitals to receive and treat patients, interrupt programmes to promote community health and prevent disease, and change the general situation of the population for the worse.
Earlier, we talked about people who are vulnerable to epidemics. Now, from the table we have created above, we can see that even more people can become vulnerable after a natural disaster. This is because natural disasters frequently affect living conditions, shelter, sanitation, and the supply of food and water, and may also cause people to move.
Group work
In small groups, remember what helps spread epidemics. Discuss and find a sentence that describes the link between natural disasters, their effects and epidemics.
Follow the example below:
Earthquakes cause people to leave their homes and live in tents and temporary shelters in crowded conditions. This helps spread respiratory infections.
Each group will work on one of the following kinds of disasters:
Earthquakes
Floods
Landslides
Storms
Tsunamis
Refugee crises
Droughts and famine
Write all the sentences the groups come up with on the flipchart or board and discuss them with the whole group.
Part 1.4.2. Dead bodies in natural disasters
After most natural disasters, there is a strong fear that dead bodies will cause epidemics. This belief is wrongly promoted by the media, as well as by some medical and disaster professionals.
Dead bodies do not cause epidemics after natural disasters!
The pressure created by these fears may lead the authorities to adopt unnecessary measures to dispose of the dead, such as mass burial or spraying disinfectant. Such actions can cause mental distress and legal problems for the relatives of those who have died.
It is very important to know that survivors are much more likely to spread disease than are the dead.
Infections and dead bodies
People who die as a result of natural disasters are normally killed by injury, drowning or fire, not infections. At the time of their death, these people are not likely to have been sick with infections that cause epidemics. Most germs that cause infections will not survive in dead bodies for more than 48 hours.
Risks to other people
The risk to the public is small because most people do not touch dead bodies. There is a risk that drinking water may be contaminated by the faeces (stools) released by dead bodies, but this risk is also only small.
Risk to body handlers
Individuals who handle human remains (bodies) are at some risk if they are in contact with blood and faeces infected by hepatitis (a liver infection), HIV, tuberculosis or gastrointestinal infections. Body recovery teams that work in dangerous places, such as collapsed buildings, may also be at risk of injury.
Safety precautions for body handlers in natural disasters
As volunteers, you may be called upon to handle dead bodies after a natural disaster. It is important to know what safety precautions you should take to avoid, and avoid spreading, infections. Observing basic hygiene will protect you from being infected during contact with blood and other body fluids.
Volunteers should take the following precautions when handling dead bodies:
- Use gloves once only and dispose of them correctly.
- Wash your hands with soap and water after handling bodies and before eating.
- Avoid wiping your face or mouth with your hands.
- Wash and disinfect all vehicles used to transport bodies as well as associated equipment and clothes.
- Face masks are not necessary but should be provided, if requested, to avoid anxiety.
- Be vaccinated against hepatitis B.
Part 1.4.3. Dead bodies in epidemics
People who die in epidemics have died because of an infection. However, most germs cannot survive long once a person has died. The majority of infectious diseases cannot be transmitted from one person to another after death. You should take the normal precautions listed above when you assist families to safely manage deaths during epidemics.
This said, there are some exceptions. They include Ebola and Marburg fever which are highly contagious after death. Special precautions must be taken when managing dead bodies in these outbreaks and it is vital to wear full personal protection equipment (PPE).
Assisting families and communities to safely manage dead bodies with dignity during epidemics requires specialized training. If an epidemic that can be transmitted after death occurs in your area, special teams will be formed to support communities.
Volunteers engaged in the management of dead bodies should understand how the society buries its dead and should identify all related risks. This matter is very sensitive for families and for the community and can be a source of conflict between them and epidemic responders. Before starting any procedure, every step in the burial process should be explained to the family. It is very important to respect the dignity of the deceased person.
Once the arrangements have been agreed and understood, the burial can be performed. No burial process should take place until agreement is obtained. Members of a safe and dignified burial (SDB) team need to possess the following skills:
- To understand the disease that is responsible for the epidemic, as well as the virus or organism that causes it and its modes of transmission.
- To know the correct procedures for handling potentially infectious dead bodies, including the donning and removal of PPE if the disease is highly infectious.
- To exercise self-discipline in following the procedures correctly in every circumstance.
- To be sensitive to the needs and beliefs of the community. They should be trained in communication and psychosocial support.
Specialised training materials are available if safe burial is required. Safe burials should only be undertaken with appropriate technical support.
Illustration 2. PPE (Personal protection equipment)
Part 1.4.4. One Health
Some human diseases result from interaction with animals and the environment. People who are in contact with animals and animal products (such as meat, milk, or dairy products) or carcasses, are at risk from diseases that animals can transmit. Insects can also transmit some diseases from animals to humans. Animals can be infectious even if they show no signs of disease.
Changes in the environment can expose both humans and animals to infectious diseases. For example, when a human population occupies a new area, it may be more exposed to diseases transmitted by wildlife. People may also be at higher risk of disease following deforestation or the expansion of industry. Environmental changes also expose animals to new infectious agents. Finally, the growth of international travel and trade allows diseases to spread easily and swiftly across the globe.
One Health is an approach that can be applied locally, nationally, regionally and globally to achieve optimal health outcomes. It takes account of the unavoidable interconnections between people, animals, plants and the environment they share. It considers the social and behavioural environment as well as the physical.
Figure 6. One Health
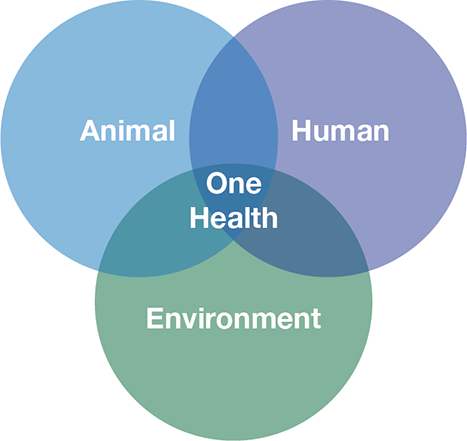
An epidemic that affects both animals and humans cannot be stopped by one sector acting alone, even if that sector makes significant efforts. Close collaboration between professionals in human and animal health is essential.
Participate
List diseases that can be transmitted from animals to humans. Do you know what actions human and animal health services take to prevent and control those diseases? What can volunteers do to support their efforts?
Volunteers might participate in the following activities:
- Support animal vaccination campaigns.
- Participate in animal disease surveillance, of both wild and domestic animals.
- Help to isolate and quarantine sick animals.
- Promote protective behaviour, for example by ensuring that people do not eat sick or dead animals and cook animal products thoroughly.
- Promote use of personal protection equipment (PPE) when in contact with animals that have highly infectious diseases.