Group 1. Faecal-oral infections
 |
Disease tools:
|
This disease group includes acute diarrhoeal diseases (including cholera) and other diseases that do not cause diarrhoea but have the same principal mode of transmission (hepatitis A and E and typhoid fever).
| Diarrhoea |
|---|
|
is when a child (or an adult) passes three or more liquid stools in a day. It can cause a child to lose so much body water and minerals that he or she dries out (dehydrates). In some cases, diarrhoea can cause death if it is not treated. |
Many children get diarrhoea. On many occasions, it can be cured simply. But sometimes it can spread and cause an epidemic. There are different kinds of diarrhoeal disease. Some take the form of watery stools; in others, blood comes out with the stools. A diarrhoeal disease called cholera is particularly severe.
How are these diseases transmitted?
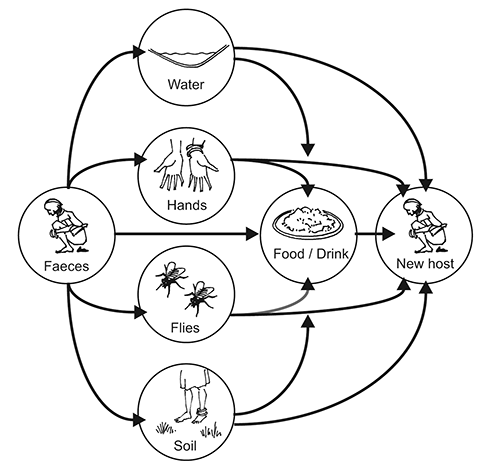
Faecal-oral transmission occurs when microorganisms from an infected stool of one person enter the mouth of another. This may occur if faeces contaminate food or the water supply or when germs are transferred from hand to mouth because the hands have touched contaminated items and have not been well washed afterwards.
Figure 14. Faecal oral transmission
What symptoms do they cause?
Children are particularly subject to severe forms of diarrhoeal disease. When children get diarrhoea, they start to have frequent loose stools. This causes their bodies to lose water and minerals. Other symptoms of diarrhoea include stomach pains, fever, cramps, nausea and vomiting. When a child loses a lot of water, he or she can become dehydrated.
In areas where it is common, many children get hepatitis A. Most will have no symptoms. In some children, the symptoms of liver disease occur: the skin and whites of the eyes become yellow and the child has fever, tiredness, abdominal pain and diarrhoea. This disease can be prevented by a vaccine. In areas where hepatitis A is rare, adults mainly get the infection and it will be more severe.
Hepatitis E causes the same symptoms as hepatitis A, but it is very dangerous for pregnant women.
Persons with typhoid fever usually have a sustained high fever. They may also feel weak, have stomach pains, a headache, or loss of appetite. A vaccine protects against typhoid fever.
Two kinds of diarrhoea are particularly severe:
- Dysentery. Blood comes out with the stools.
- Cholera. This disease causes more severe symptoms and very watery stools that look like “rice water”.
How do we prevent epidemics?
Epidemics of faecal-oral infections can be prevented by some simple actions:
- Hygiene. Wash hands with soap at critical times, especially after going to the toilet, after cleaning children’s bottoms, and before preparing food and eating.
- Drink only clean and safe water. Where safe drinking water (including bottled water) is unavailable, boil or filter water or treat it with chlorine, and store it in clean containers.
- Eat safe food. Wash vegetables and fruits with safe water, thoroughly cook meat and other animal products, store food in clean conditions and reheat food before eating it.
- Build appropriate sanitation facilities (latrines) in the community. This will help reduce the likelihood that stools will contaminate water or food. Special care should be taken with children’s stools, which should be properly disposed of in the latrine or buried.
- Breastfeed babies during the first six months of life. Exclusive breastfeeding will protect infants and prevent severe forms of diarrhoea. Breastfeeding should not be interrupted when a child is sick because it is not the cause of the diarrhoea and has a continuous beneficial effect on survival.
How to deal with cases of these diseases?
When dealing with diarrhoea cases, the key point is to replace the water and minerals the sick person is losing. It is vital to correct dehydration. This is done by detecting diarrhoea early and giving the person water, sugar and salts. These can take the form of an oral rehydration solution (ORS), made from a packet, or home-made fluids such as rice water or soup or breastfeeding. Zinc supplements reduce the duration of diarrhoeas. In cases of severe dehydration or shock it is necessary to give intravenous fluids to the affected person.
Hepatitis A and E usually cause mild infections in children, but in adults, especially pregnant women, the condition is dangerous and may require hospitalization.
Typhoid fever is treated with antibiotics.
How to detect an epidemic?
We suspect an epidemic of diarrhoea when many more people than usual, especially children, have diarrhoea and are dehydrated at one time, and cases are more severe than normal.
We suspect cholera when adults, as well as children, have severe diarrhoea and dehydration and some of them die as a result.
An epidemic of hepatitis is suspected when many people have symptoms of liver disease (e.g., yellowing of the eyes).
An epidemic of typhoid fever is suspected when more people than usual have high fever without symptoms of respiratory diseases.
Early detection of an epidemic is more likely when there is disease surveillance. Early detection permits a prompt response which can save many lives.
| The epidemic |
|---|
|
Who? Severe diarrhoeas, especially cholera, can affect anyone, including adults. Severe forms of hepatitis mainly affect adults. Where? When? Why? |
How to deal with an epidemic?
If an epidemic caused by faecal-oral infection occurs in your community, here are some things that should be done:
- Build trust with members of the community.
- Involve the community in efforts to control the epidemic.
- Familiarize yourself with the community’s culture.
- Find out the source and cause of the epidemic disease (unsafe water, inappropriate latrines, unsafe hygiene practices).
- Treat water (by boiling or filtering it or treating it with chlorine) and store water safely.
- Identify cases of the disease.
- Care for dehydrated children at home with ORS or home-made fluids (rice water, soup, breast milk) and zinc supplement.
- Refer very sick and dehydrated children to health facilities.
- Promote hygiene in local communities and among families.
- Establish community oral rehydration points for early treatment and referral.
- Apply safety procedures for handling and burying dead bodies.
Learn
It is very important to recognize dehydration in children when looking for cases of diarrhoeal disease. This skill will help you to decide who should be treated with an ORS at home and who should be referred to the health centre or hospital.
The table below will help you recognize dehydration and its severity.
Table 4. Stages of dehydration
| Dehydration stage | Signs | Treatment |
|---|---|---|
| No dehydration | Skin goes back normally when pinched, thirst has subsided, urine has been passed, pulse is strong. | ORS at home; zinc supplement in children up to 15 years old. |
| Moderate dehydration | Restlessness and irritability, sunken eyes, dry mouth and tongue, increased thirst, skin goes back slowly when pinched, decreased urine, decreased tears, depressed fontanels (soft membrane on head) in infants. | ORS plus very close surveillance; zinc supplement in children up to 15 years old. |
| Severe dehydration | Lethargy or unconsciousness, very dry mouth and tongue, skin goes back very slowly when pinched (“tenting”), weak or absent pulse, low blood pressure, little or no urine. | In a health facility or in a hospital: IV therapy plus antibiotics plus ORS; zinc supplement in children up to 15 years old. |
What can volunteers do?
Volunteers can play a critical role in communicating with and mobilizing communities. They can encourage people to change their behaviour and adopt safe personal and domestic hygiene practices. They can help teach caregivers about oral rehydration and the importance of breastfeeding. They can advise parents and families to take very sick children to health centres.
Volunteers can look for new cases of infection and inform staff at the health centre. They can take part in investigating the source and cause of the epidemic.
Most importantly, volunteers can:
- Help detect cases of disease in their local communities.
- Help families to identify warning signs of dehydration, especially in children.
- Refer people with severe dehydration and fever, or people at high risk such as elderly or pregnant women.
- Talk to members of affected communities to understand their concerns, fears and typical water, sanitation, hygiene and community care practices.
- Help to mobilize the community to take action to protect itself, and influence the community to change harmful forms of behaviour (using BCC).
- Show mothers and caregivers how to prepare oral rehydration solution (ORS) for dehydrated children.
- Set up and run oral rehydration points (ORPs) in affected communities. See IFRC ORP guideline/ORP training manual.
- Alert the health authorities to new cases or outbreaks.
- Provide psychosocial support to sick people and their families.
- In a major epidemic, work with other Red Cross Red Crescent partners in cholera treatment centres or mobile hospitals.
Participate
Discuss within your group whether an epidemic might be caused by a faecal-oral infection. Look at the disease tools for faecal-oral infections and select the action and message tools for each. Discuss with your facilitator the similarities and differences between the tools for each disease in this category. Take note that the same method is used to prevent all the diseases in this category.