17. Measuring mid upper arm circumference (MUAC)
Overview
What is a MUAC test?
MUAC is a simple measurement that can be used to identify children (six months to five years) who have malnutrition and are at risk of dying. It uses a coloured tape that is wrapped around the left upper arm. Parents and carers can be trained to measure the MUAC.
Children whose arm circumference falls within the red or yellow indicator on the coloured tape (see table below) should be referred to the nearest health or nutrition centre.
What to do and how to do it
Preparing to screen for malnutrition
- Find out which health facilities or centres treat malnourished children in your area. (Some facilities only address severe acute malnutrition (SAM) and not moderate acute malnutrition (MAM)).
** You should only begin screening for malnutrition IF there are appropriate treatment centres, validated for quality assurance by a health professional, to which to refer people **
- Inform the community and parents that MUAC tapes identify children who are malnourished.
- Inform the community that thin, weak children who are not growing well can obtain treatment without cost and indicate where they can access this service.
- Find out the local word for a child who is very thin and use it to help find cases.
Measuring MUAC
- Mid upper arm circumference (MUAC) screening can be done on anyone over the age of six months and is commonly used for children six to 59 months (six months up to five years). The size of the MUAC tape is different for different age groups. Make sure you are using the correct size of MUAC for the age group you are measuring.
- Use MUAC to measure children between six months and 59 months of age, especially those who are sick, thin or weak.
- Explain the procedure to the child’s mother or caregiver.
- Ensure that the child is not wearing any clothing on his or her left arm.
- If possible, the child should stand straight and sideways to the measurer.
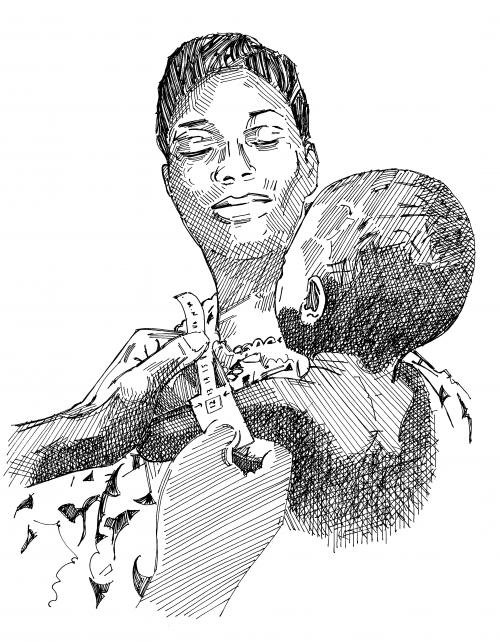
- Bend the child’s left arm at 90 degrees to the body.
- Find the mid-point of the upper arm. The mid-point is between the tip of the shoulder and the elbow.
- Mark with a pen the mid-upper arm point.
- Ask the child to relax the arm so it hangs by his or her side.
- Using both hands, place the MUAC tape window (0 cm) on the mid-point.
- While keeping the left hand steady, wrap the MUAC tape around the outside of the arm with the right hand.
- Feed the MUAC tape through the hole in the tape while keeping the right hand planted on the arm.
- Pull the tape until it fits securely around the arm while keeping the right hand steady on the child’s arm.
- Read and record the measurement at the window of the MUAC tape to the nearest millimetre (mm).
- If a child has a MUAC coloured yellow or red on the tape, a referral to the nearest health or feeding centre should be made.
Making referrals
- Refer children that have a red or yellow MUAC to the appropriate treatment centre, identified when you were preparing for screening.
| Colour | Nutritional status | Action |
| Red | Severe | Refer to the nearest health facility that provides therapeutic feeding. |
| Yellow | Moderate | Refer to the nearest health or nutrition centre that provides supplementary feeding (if available). |
| Green | Healthy | Encourage the carer to continue with healthy hygienic care and feeding practices, and to return if the child becomes sick or weaker. |
Social mobilization and messaging
- Explain the MUAC arm measurement to caregivers. Tell them if it shows their child(ren) is/are malnourished and should receive treatment.
- Encourage caregivers to seek health treatment quickly if their child is malnourished. Tell them that treatment will enable the child to grow well, prevent stunting, and help the child to avoid diseases later in life.